By Sasha
’24
New scientific research has revealed the ubiquitous and significant effect of gut microbiome health on a person’s mental wellbeing. This relationship was given a title of the ‘gut brain axis’, referring to the bidirectional communication between the brain and gut. “[The] communication occurs through neural, inflammatory, and hormonal signalling pathways.” said by Dr. Ghannoum in Woman’s World Magazine, a director at University Hospitals Cleveland Medical Center. Essentially, your brain and gut are interrelated.
The new studies carried out by researchers at Oxford Population Health was aimed to reveal a correlation between gut microbiota and symptoms of depression. It was concluded that some bacteria showed a potential impact in the way people produce neurotransmitters. This was especially significant in neurotransmitters linked to depression such as glutamate which maintains balance in the gut microbiome.
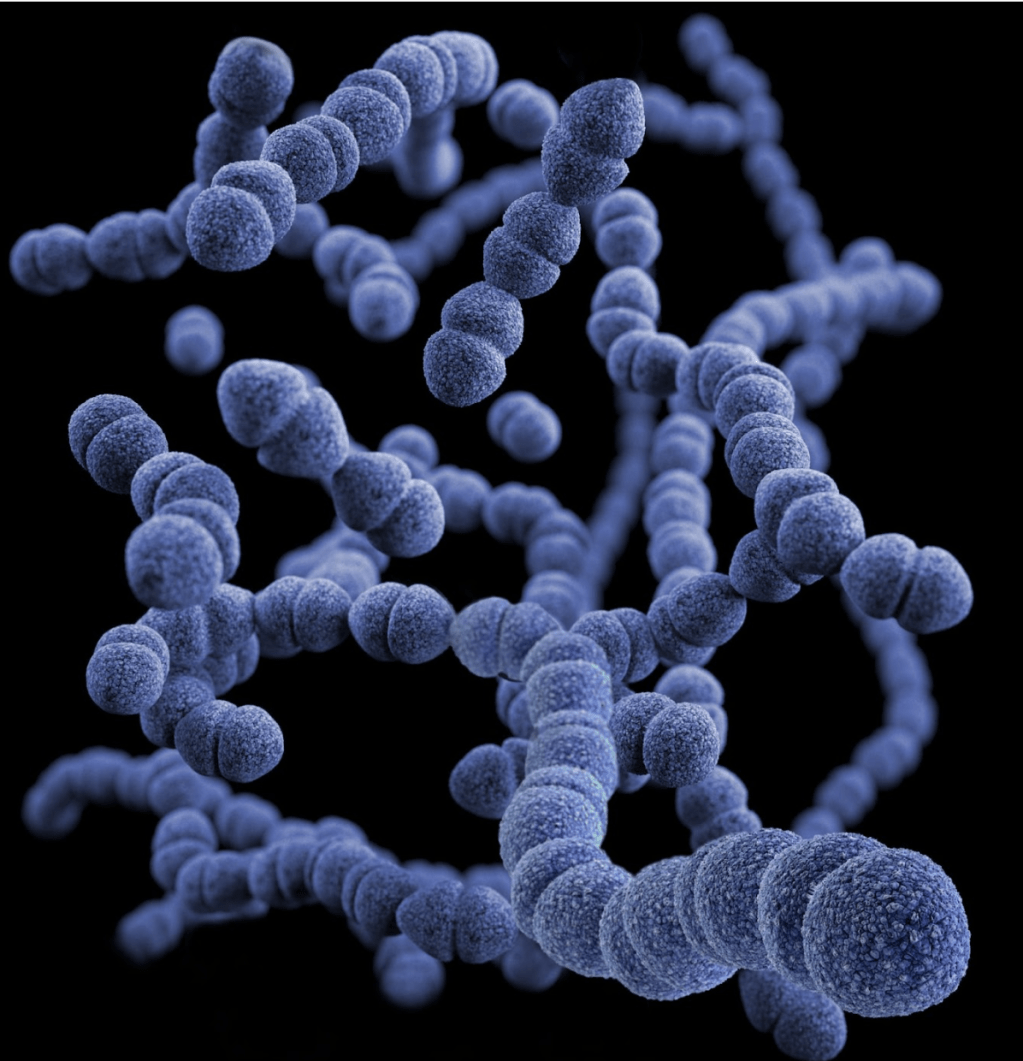
A microbiome is inhabited by trillions of microorganisms composing a dynamic system involved in health and illness. The composition of an organism’s gut microbiota is unique to every individual and tends to stay relatively stable throughout life, however daily short lasting fluctuations have been observed through research. Diet and nutrition can be a key modifiable factor that influences the composition of the gut microbiota, indicating the potential for therapeutic dietary methods to be used to control microbial diversity, composition, and stability.
Certain types of bacteria in higher or lower concentrations have been seen to impact the likelihood of experiencing symptoms of depression. Another study in Rotterdam investigated 1,000 Euopeans and another study investigated 3,000 people in Amsterdam from different ethnic groups. The results from this study found that patients showing higher levels of Lachnospiraceae and the genus Eggerthella bacteria were more prone to depressive symptoms; whereas lower levels of the bacteria family Ruminococcaceae were also linked to depressive symptoms. The levels of certain bacteria in a person’s gut microbiome can be somewhat controlled by a person’s diet and nutrition choices.
A study done at CalTech, a science and engineering institute, has shown that an estimated 90% of serotonin is produced in the digestive tract. Serotonin makes you feel “more focused, emotionally stable, happier and calmer” according to Cleveland Clinic. The study also revealed that “Altered levels of [the] serotonin [produced] from the gut] have been linked to diseases such as irritable bowel syndrome, cardiovascular disease, and osteoporosis.” Considering how consequential the impacts of gut microbiota change is on chronic conditions, is there something that we as individuals could do to control our microbiota and improve our physical and mental health?
Harvard School of Public Health recommends a diet rich in fibre. “Dietary fibre can only be broken down and fermented by enzymes from microbial living in the colon”, and as a result of this fermentation, short fatty acid chains (SFAC) are released, in turn lowering the pH of the colon. This change of pH creates a more acidic environment and limits the growth of some harmful bacteria. This reduction of bacteria has been researched by Harvard to “simulate immune cell activity and maintain normal blood levels of glucose and cholesterol”. Some types of food that also support the increased levels of SFAC are prebiotic foods such as “fruits, vegetables, beans, and whole grains like wheat, oats, and barley”(Harvard). Though, increasing an individual’s consumption of these prebiotic foods can cause bloating and stomach pain. It is important to implement an increase in these foods gradually.
By making simple changes to your diet, such as adding more fibre into your daily sustenance, as previously mentioned can help to mitigate the negative effects that an unbalanced gut microbiota can have on not just your physical health, but mental health.The results of this research could provide innovative pathways into thinking about and combating symptoms of depression, which is a major step we have into understanding mental health today. One way to move forward knowing this information is trying to maintain a healthy gut microbiome through supporting and supplementing your diet through nutrition.
Bibliography
California Institute of Technology. (2016). Microbes Help Produce Serotonin in Gut. [online] Available at: https://www.caltech.edu/about/news/microbes-help-produce-serotonin-gut-46495#:~:text=Although%20 serotonin%20 is%20 wheel%20 known.
Cartusciello, Jenna. “Why Better Gut Health Equals Better Mental Health — and the Best Ways to Improve Both, according to Experts.” Woman’s World, 23 Nov. 2022, www.womansworld.com/posts/health/gut-health-mental-health-gut-brain-axis.
Cross, Paul Ian. “Depression and Gut Bacteria: What Is the Link?” Www.medicalnewstoday.com, 12 Dec. 2022, https://www.medicalnewstoday.com/articles/do-gut-bacteria-play-a-role-in-depression
“Experts Explain Why Gut Is Called “the Second Brain.”” The Indian Express, 10 Dec. 2022, indianexpress.com/article/lifestyle/health/mental-health-gut-8262656/. https://indianexpress.com/article/lifestyle/health/mental-health-gut-8262656/
Harvard T.H. Chan. “The Microbiome.” The Nutrition Source, 4 Sept. 2019, www.hsph.harvard.edu/nutritionsource/microbiome/.
Health, Oxford. “Your Gut Bacteria May Play a Key Role in Whether You Have Symptoms of Depression — Nuffield Department of Population Health.” Www.ndph.ox.ac.uk, 6 Dec. 2022, https://www.ndph.ox.ac.uk/news/the-bacteria-living-in-your-gut-may-play-a-key-role-in-whether-or-not-you-have-symptoms-of-depression
J. Deters, Brett, and Mir Saleem. “The Role of Glutamine in Supporting Gut Health and Neuropsychiatric Factors.” Food Science and Human Wellness, vol. 10, no. 2, Mar. 2021, pp. 149–54, https://doi.org/10.1016/j.fshw.2021.02.003.
Mosbergen, Dominique. “Gut Bacteria Are Linked to Depression.” WSJ, 6 Dec. 2022, https://www.wsj.com/articles/gut-bacteria-linked-to-depression-11670342342
Leeming, E.R., Johnson, A.J., Spector, T.D. and Le Roy, C.I. (2019). Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6950569/
Publishing, Harvard Health. “The Gut-Brain Connection.” Harvard Health, 19 Apr. 2021, www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection#:~:text=A%20 troubled%20 intestine%20can%20 send.
Rajabzadeh, Djawad, et al. “Gut Microbiome-Wide Association Study of Depressive Symptoms.” Nature Communications, vol. 13, no. 1, 6 Dec. 2022, p. 7128, https://www.nature.com/articles/s41467-022-34502-3
Leave a comment